- Home
- Trend
- Weight Loss Strategies
- Acne Tips
- Hair Health Information
- Blemish Removal Tips
- Acne Scar Removal Tips
- Muscle Building Techniques
- Intimate Care Tips
- Postpartum Intimate Care
- Eye Bags Wiki
- Tips for Face Slimming
- Secret of Permanent Hair Removal
- Breast Enlargement Tips
- Cure to Snoring
- Marionette Lines
- Skin-Tightening Secrets
With today’s fast-paced lifestyle, more and more people are struggling with sleep apnea, a serious sleep disorder. Sleep apnea doesn’t just affect your sleep quality — it can also trigger a range of chronic health problems. Recognizing the signs early and taking action is essential.
1. How Serious Is Sleep Apnea? Poor Sleep + Higher Risk of Chronic Disease

According to Hong Kong’s Hospital Authority, over 100,000 people suffer from varying degrees of sleep apnea. Yet, many are unaware they even have it. Research shows about 4% of men and 2% of women in Hong Kong are diagnosed with sleep apnea, most commonly middle-aged men between 30 and 60. Among those over 65, 1 in 4 people may be affected.
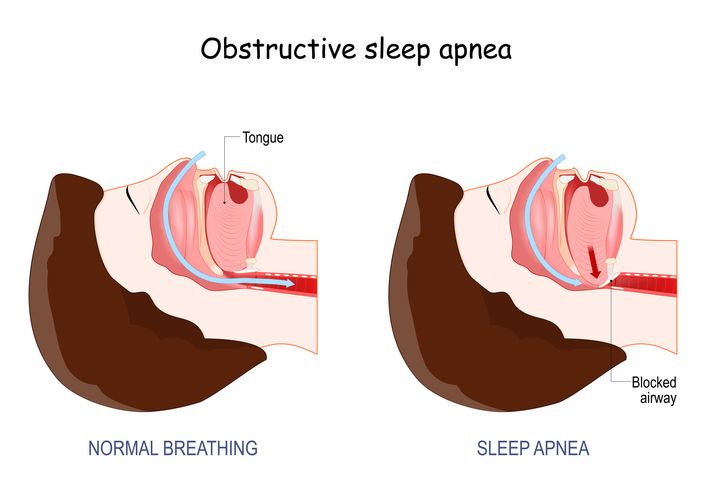
So why is it dangerous? During sleep, the upper airway becomes blocked or collapses due to relaxed muscles, preventing normal airflow. This lack of oxygen causes repeated awakenings throughout the night. As a result, patients often wake up extremely tired, as if they didn’t rest at all — impacting their work and daily life.
Studies also link sleep apnea with a higher risk of chronic illnesses such as diabetes. Prolonged oxygen deprivation can damage major organs, raising the chances of developing:
• Hypertension
• Cardiovascular disease
• Heart failure
• Stroke
• Coronary artery disease
• Pulmonary hypertension
• Impaired lung function
• Polycythemia (abnormal red blood cell increase)
In severe cases, oxygen deprivation during sleep can even lead to sudden death.
2. The 3 Main Types of Sleep Apnea — Which One Do You Have?
Understanding the type of sleep apnea is key to treatment. The three primary types are:
1. Obstructive Sleep Apnea (OSA)
The most common type, accounting for about 90% of cases. It’s caused by airway narrowing or blockage during sleep, often due to enlarged tonsils, nasal allergies, an abnormal uvula position, or the tongue obstructing the throat. Patients may experience multiple breathing pauses that disrupt deep sleep.
2. Central Sleep Apnea (CSA)
Caused not by physical obstruction but by the brain failing to send proper breathing signals. This is often linked to heart disease, stroke, or brain injury.
3. Mixed Sleep Apnea
A combination of obstructive and central apnea, where both airway blockage and faulty brain signals occur. This makes treatment more complex, often requiring multiple approaches.
免費體驗
Fotona 4D NightLase Snoring Treatment
1 Minute Self-Registration
Date should not be before minimal date
3. 9 Common Symptoms of Sleep Apnea
Because of repeated interruptions to sleep and low oxygen levels at night, patients often experience:
1. Loud snoring with pauses in breathing
2. Difficulty concentrating
3. Memory decline
4. Persistent morning fatigue
5. Insomnia or restless sleep
6. Excessive daytime sleepiness
7. Morning headaches
8. Irritability or depression
9. Reduced sexual function
ENT specialist Dr. Chan Kin-Ming reminds us: snoring does not always equal sleep apnea. A normal person may experience fewer than 5 episodes of breathing pauses per hour. But:
• 5–15 times per hour = mild sleep apnea
• 16–30 times per hour = moderate
• Over 30 times per hour = severe
4. 6 Ways to Manage Sleep Apnea: Lifestyle + Medical Treatments
Since sleep apnea is a complex condition, treatment usually requires a combination of lifestyle changes and medical support. Here are 6 common options:
1. Change Sleep Position & Manage Weight
Sleeping on your back increases airway blockage risk. Side-sleeping helps keep the airway clear. Weight loss is also key, as excess fat around the neck can worsen obstruction.
2. Quit Smoking, Alcohol, and Sleeping Pills
Smoking irritates the airway and increases mucus. Alcohol and sedatives relax throat muscles, raising the chance of airway collapse. Quitting or reducing intake improves symptoms.
3. Dental Appliances (Oral Devices)
For mild cases, customized oral devices can reposition the jaw and prevent the tongue from blocking the airway.
4. CPAP Machine (Continuous Positive Airway Pressure)
The mainstream treatment for all severity levels. CPAP delivers pressurized air to keep airways open. While not a cure, it’s highly effective for symptom control — though some patients find it uncomfortable.
5. Positional Therapy (Headbands or Pillows)
Devices like side-sleep headbands or contour pillows encourage side-sleeping, reducing airway collapse from the tongue or uvula.
6. Surgery
Options include widening the airway, removing blockages, or correcting structural issues. Surgery may help in severe cases but comes with risks and recurrence possibilities, so it should be carefully considered with a doctor.
5. Fotona 4D NightLase Snoring Treatment — A Faster, Non-Invasive Option
Beyond traditional methods, there’s an advanced treatment worth noting: the Perfect Medical Fotona 4D NightLase Snoring Treatment.
Using patented NightLase™ laser technology, this treatment stimulates collagen in the oral tissues, tightening and reshaping them to keep the airway clear. It’s:
• Non-invasive & painless
• Targets snoring causes like enlarged tonsils, uvula, muscle relaxation, or nasal issues
• Delivers quick results, with improvements often seen after the very first session
• Long-lasting, with effects that can last up to 9 months
Compared to traditional methods, this offers a faster, safer, and more comfortable solution — with no downtime required.
Looking for an effective, safe way to stop snoring and improve sleep apnea? Try the Perfect Medical Fotona 4D NightLase Snoring Treatment. First trial is free — book your appointment online today!
Get Your First Trial: Perfect Medical Fotona 4D NightLase Snoring Treatment免費體驗
Fotona 4D NightLase Snoring Treatment
1 Minute Self-Registration
Date should not be before minimal date
FAQ

Who is most at risk of sleep apnea?
Elderly individuals (1 in 10 over 70), middle-aged men (2–8x more likely than women), obese individuals (up to 70% risk), people with short jaws, enlarged tonsils, nasal structural issues, or existing conditions like heart disease, stroke, and diabetes. Smokers, heavy drinkers, and sedative users are also at higher risk.
How is sleep apnea diagnosed?
Through a polysomnography sleep study, which measures brain waves, airflow, and snoring. This can be done in hospitals or at home using specialized devices or sleep-monitoring rings. The Epworth Sleepiness Scale is also commonly used for self-assessment.
Does treatment require long-term commitment?
Yes. CPAP, oral appliances, and lifestyle changes usually require ongoing use. Regular follow-ups and sleep assessments help ensure lasting improvements.
Can medication treat sleep apnea?
Not effectively. There’s no widely recognized medication for curing sleep apnea. Drugs may ease symptoms temporarily but aren’t a primary solution. Mechanical and behavioral therapies remain the mainstay.
Can sleep apnea heal on its own?
Unlikely. Professional evaluation and treatment are strongly recommended to avoid long-term complications.